By: Aleisha Robinson with SGJC Student News Network
The opioid crisis continues to devastate communities in Maryland, but what if the best way to save lives isn’t through rehab or prison, but by providing clean needles?
That’s the premise behind harm reduction, a public health approach that focuses on minimizing the negative effects of drug use instead of criminalizing it.
In cities like Baltimore, where overdose deaths have spiked to some of the highest in the country, advocates say strategies like distributing naloxone to reverse overdoses, offering syringe services, and opening overdose prevention centers, where people can use drugs under medical supervision, could be the key to saving lives. But even as experts agree on these evidence-based solutions, funding and legal barriers continue to stand in the way, say advocates.
In January, State Senator Shelly Hettleman reintroduced Senate Bill 83, known as the Public Health - Overdose and Infectious Disease Prevention Services Program. This legislation sought to authorize community-based organizations, with the approval of the Maryland Department of Health, to establish overdose prevention centers, providing supervised locations for the consumption of pre-obtained drugs.
These programs would offer sterile needles, administer first aid, and deliver other health services. The bill proposes allowing up to six programs, with a preference for two each in urban, rural, and suburban areas.
But Senate Bill 83 stalled in committee —just like similar proposals have in previous years. According to Senator Hettleman, political hesitancy continues to outweigh community needs.
“Even with education, touring facilities, and having expert panels, there are many on the committee who simply have a philosophical difference in how this issue should be tackled,” said Hettleman.
That difference, she believes, is rooted in stigma.
“Unfortunately, there is still a perception that we can arrest our way out of this —or at least some feel as if opening an ‘overdose prevention site’ encourages and promotes drug use,” Hettleman added. “It’s similar to people who are opposed to handing out condoms and birth control saying that will encourage promiscuity.”
The Overdose Epidemic in Baltimore
Baltimore has had the highest overdose rate of any major metropolitan city for over five years. According to the Baltimore City Health Department, from 2024 -2025, there were a total of 1,549 Overdose Deaths, 1,257 Deaths Related to Any Opioids and 1,130 Deaths Related to Fentanyl.
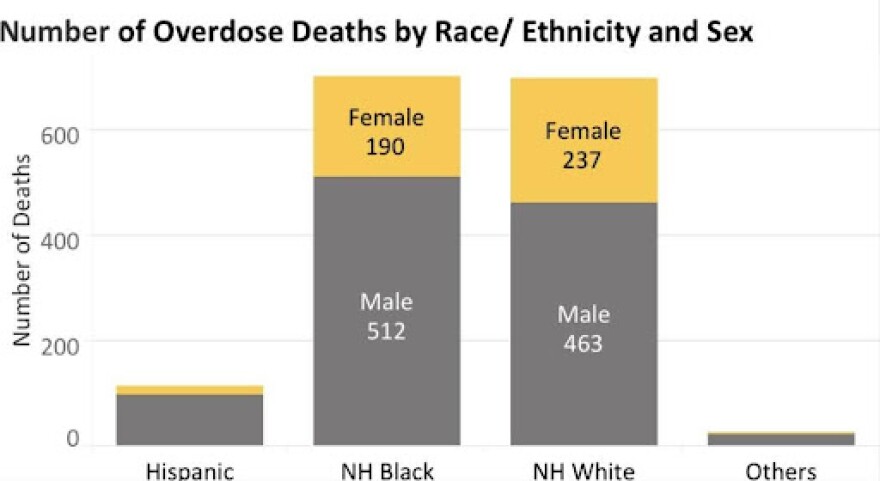
There was a significant nearly 30% drop in overdoses in Baltimore in 2024, mirroring decreases across the country, but according to data from the City’s health department, Black residents —especially men between the ages of 35 and 54 —continued to be disproportionately affected.
These patterns highlight how the crisis persists along racial and socioeconomic lines, underscoring the urgency of implementing proven public health interventions, say researchers and experts.
“Older Black men have been disproportionately affected by overdose deaths in Baltimore City since around 2015,” said Jay Unick, a professor at the University of Maryland. “Their rising death rates went largely unnoticed for too long.”
Number of Overdose Deaths by Place of Occurrence (April 2024- March 2025)

As Baltimore struggles to curb its overdose crisis, the city is also preparing to receive more than $668 million through lawsuits against pharmaceutical companies for their role in the epidemic. Because Baltimore opted out of a national settlement and sued on its own, it’s set to receive six times more than it would have otherwise, according to Baltimore city officials.
City officials like Sara Whaley the Executive Director of Overdose Response say these funds — now being paid into the Baltimore City Opioid Restitution Fund — are a once-in-a-generation opportunity to invest in overdose prevention and treatment care at the community level.
“So really focusing the dollars on going into the community and addressing the overdose crisis rather than spending them on other things,” said Whaley.
Whaley says the intent is to ensure resources go where they’re needed most — into life-saving services like harm reduction, treatment access, and support for people who use drugs.
She added that funds should support programs grounded in evidence and shaped by the input of people with lived experience, not diverted toward law enforcement or punitive measures.
“That’s what these dollars are for — to actually reduce suffering and save lives.”
Support for harm reduction in Baltimore City
Baltimore has long been on the vanguard of the harm reduction movement. Programs like the Baltimore City Health Department’s needle exchange have been operating since the 1990s, and local organizations continue to innovate.
Hop-On Harm Reduction, run by Johns Hopkins University, provides essential services such as needle exchange, wound care, hygiene products, and overdose supplies like Narcan and fentanyl test strips.
“Our reach and distribution have been extensive and we have also established rapport with many participants who now have a stigma-free place to obtain services,” said Karin Tobin, faculty advisor to the program.
While Maryland state government is largely supportive and funds many harm reduction services, she noted that, “Having a funded consumption site would be great” to further improve the city’s harm reduction infrastructure.
Mayor Brandon Scott has expressed his commitment to harm reduction as part of a broader strategy to save lives.
In a 2023 executive order, Scott mandated that the city increase naloxone distribution and training, “ensuring that both first responders and community members have the tools they need to save lives.”
He emphasized the need to treat addiction as a public health issue rather than a criminal one, stating that the city must “reduce overdose deaths and empower individuals to seek long-term treatment when they are ready.”
Mayor Scott has publicly stated his strong interest in bringing overdose prevention sites to Baltimore City.
But, despite his administration’s push for this approach, it’s an uphill battle at the state legislative level. “No politician wants to be the one who ‘brought sanctioned drug use’ to their district,” said Logan Hullinger, an independent journalist covering addiction, drug policy and the harm reduction movement in Baltimore.
“Even if overdose prevention centers are proven to work — with zero deaths in those facilities — it’s still viewed as political suicide. Voters hear ‘safe drug use’ and think it’ll tank their property value,” said Hullinger.
Success of OPCs
According to an analysis from the National Institutes of Health (NIH), OPCs have been successfully introduced in Canada, Australia, and parts of Europe, where they have consistently proven to reduce overdose deaths and improve public health outcomes.
In the U.S., New York City opened the first officially sanctioned OPCs in 2021. The program has seen remarkable success, with over 600 overdose reversals reported within the first year of operation, according to the city's Department of Health.
No deaths have occurred at any of the officially sanctioned OPCs globally, a strong indicator of their effectiveness in saving lives, say advocates. In addition to reducing overdose deaths, these centers provide an opportunity for individuals to access essential health services such as medical treatment, addiction counseling, and housing assistance.
Moreover, studies from Canada and Europe indicate that OPCs not only reduce fatalities but also reduce public drug use and improve the surrounding community's safety by lowering rates of discarded needles and other drug-related litter.
Looking ahead
Baltimore has more money than most cities to fight the opioid crisis because of the remarkable success of its legal strategy to sue companies on its own. . But even with that advantage, political hesitation, and fear of public backlash could prevent the city from pursuing overdose prevention centers.
That’s where coordination becomes crucial. Sara Whaley shared her hopes for the newly created role under the mayor’s executive order — a position meant to serve as a central point of connection between city agencies and the community. She emphasized the importance of building trust and collaboration as the city moves forward in its commitment to partnership and progress.

So far, the city has received $115 million, with the rest expected by the end of 2025. Much of the money already allocated has gone to expanding existing harm reduction services run by organizations like Charm City Care Connection and Bmore POWER. But not everyone sees that as enough.
“Expanding access to MOUD (medications for opioid use disorder), recovery services, and harm reduction is critical, but not sufficient to curb the overdose crisis,” said Unick.
While evidence shows that interventions like naloxone distribution and safe consumption sites can save lives, alone, they won’t reduce overdose rates substantially, says Unick.
His reason, “people often use alone, feel more comfortable using at home or are unable to get to an OPS.”
Right now, no public plan exists to fund overdose prevention centers with the restitution money — partly due to ongoing legal barriers at the state level.
Without a shift in policy, advocates worry the city could fall short of transformative change.
“Safe consumption facilities offer an important layer of protection. They provide a supervised environment where people can use drugs without dying and serve as points of connection to services,” said Unick.
“Still, even in cities like Vancouver, Canada where such facilities are well-established, have high overdose rates. There is no single solution to this crisis; comprehensive, multi-pronged approaches are essential,” he added.


